FeNO measurement during pregnancy

Background
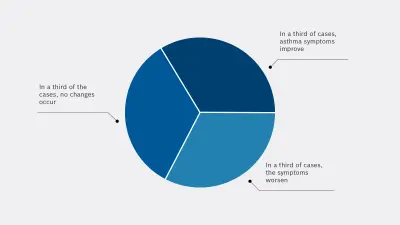
Asthma is considered the most common chronic disease in pregnancy.1 Its prevalence is estimated to be at 4-8%.1 The physiological changes that occur during pregnancy, such as an increased metabolic rate and the associated increase in oxygen consumption, can influence the progression of asthma both positively and negatively.2,3
Up to 45% of expectant women with asthma experience moderate to severe exacerbations during pregnancy that require medical intervention.4 The exacerbations during pregnancy present a major clinical problem that can lead to maternal and fetal morbidity and mortality in pregnant asthmatic women.3
Risk factors for exacerbations:

Exacerbations are a clinical problem not only for expectant mothers, but also for the fetus. Taking oral steroids and severe asthma are associated with preterm birth. This may be due to maternal hypoxia, the effects of maternal inflammation and/or changes in uterine smooth muscle function. In addition, women with exacerbations are three times more likely to have a baby with low birth weight than asthmatics who do not experience exacerbations.
This means that preventing exacerbations during pregnancy can also lead to improved perinatal outcomes.4
Recommendations for pregnant asthmatics
In early pregnancy
Asthmatic women should be offered counseling and an explanatory consultation that focuses on continued therapy with the goal of good asthma management.6 The rationale is that poorly controlled asthma and exacerbations pose a greater risk to the baby than current asthma treatments.6
During pregnancy
Asthmatics should receive close medical monitoring during pregnancy. In addition to an analysis of the patient’s case history, clinical examination and pulmonary function parameters, FeNO measurement provides a means of monitoring the allergic airway inflammation underlying asthma.6
Benefits of FeNO measurement
FeNO measurement involves measuring the biomarker nitric oxide (NO) in a standardized manner, as fractional exhaled NO (FeNO) in exhaled breath. Elevated FeNO readings indicate an inflammation of the lungs. Appropriate anti-inflammatory therapy, usually in the form of inhaled corticosteroids (ICS), can help to counteract a worsening of the condition at an early stage.
An Australian study group at the University of Newcastle monitored pregnant asthmatics and subsequently their newborn infants up to preschool age. They were able to show that the expectant asthmatics whose therapy was monitored during pregnancy with the help of regular FeNO measurements experienced less frequent exacerbations.7 In fact, they observed a 50 percent reduction in attacks.
Furthermore, their newborn infants were less likely to develop respiratory problems. It was found that their children were significantly less likely to be diagnosed with early onset asthma by around 43 percent.8

FeNO measurement is nowadays a recognized standard diagnostic procedure that is fast, easy to use and non-invasive.
In pregnant asthmatics, it has also been shown to reduce the risk of exacerbations as well as the development of early onset asthma in their children. FeNO measurement thus makes an important contribution to the health of mother and baby.
1 Kwon HL, et al. Immunol Allergy Clin North Am. 2006; 26: 29-62.
2 GINA Report 2019, Global Strategy for Asthma Management and Prevention (https://ginasthma.org/gina-reports/)
3 Shebl E, Chakraborty RK. Asthma in Pregnancy (https://www.ncbi.nlm.nih.gov/books/NBK532283/)
4 Murphy VE. Breathe (Sheff). 2015; 11(4): 258-267.
5 Giles W, Murphy V. Obstet Med. 2013; 6: 58-63.
6 Buhl R. et al. S2k-Leitlinie zur Diagnostik und Therapie von Patienten mit Asthma. 2017
7 Powell H, et al. Lancet. 2011; 378: 983-90.
8 Morten M, et al. J Allergy Clin Immunol. 2018; 142(6): 1765-1772.e4.
This website contains general product information about the Vivatmo system from Bosch. Not all products and their functions mentioned here are approved in every regional market. For a detailed description of the products and features as well as information on intended and safe use, please refer to your locally authorized Bosch distribution partner and the instructions for use that are valid for your country.


